












Aliqu justo et labore at eirmod justo sea erat diam dolor diam vero kasd
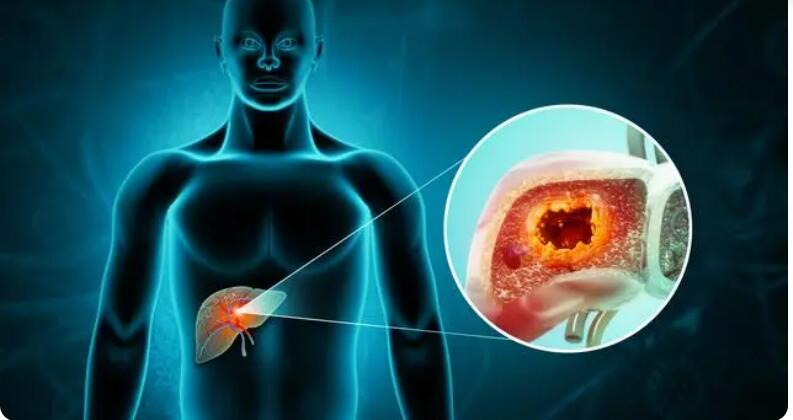
Sets of questions, organized by topic, that cancer patients may want to ask their doctors or other members of their health care team to learn more about ...
© ask cancer. All Rights Reserved.